
A retrospective cohort study comparing reconstructive techniques and outcomes in post-mastectomy triple negative breast cancer patients
Introduction
Triple negative breast cancers (TNBC), defined by the lack of expression of estrogen receptor (ER), progesterone receptor (PR), and overexpression of human epidermal growth factor receptor 2 (HER2) gene, account for 10% to 20% of invasive breast cancers (1). This breast cancer subtype more commonly occurs in patients under the age of 40 years and of African American or Hispanic ethnicity (2). Compared to other breast cancer types, TNBC is associated with the worst prognosis as there are no targeted systemic therapies given the lack of receptor expression (3,4). Prior studies have suggested a higher risk of locoregional recurrence and distant metastasis in TNBC patients who undergo breast-conserving surgery (BCS) (5,6). Previous reports have stated that patients with TNBC who were candidates for BCS opted to undergo mastectomy instead, although there is no evidence that biomolecular subtype of breast cancer should influence type of surgical treatment (4,7,8). Furthermore, a recent systematic review found no evidence of a detrimental effect of BCS compared with mastectomy on locoregional recurrence or distant metastasis in TNBC patients (4).
Immediate or delayed breast reconstruction confers psychological benefits and improvements in quality of life, and has become increasingly common following mastectomy for breast cancer (9). Recent reports suggest that immediate breast reconstruction is oncologically safe following resection of invasive breast cancer (10,11), with no differences in cancer burden in TNBC versus non TNBC patients (12). Interestingly, Kneubil et al. reported triple-negative receptor status to be an independent risk factor for locoregional recurrence in TNBC patients who elected for mastectomy with breast reconstruction (13).
Implant-based breast reconstruction (IBR) is a safe technique with favorable outcomes, minimal morbidity, and short operative times (14). Alternatively, autologous breast reconstruction (ABR) can safely be performed using microvascular free tissue transfer or pedicled locoregional flap transfer. Multiple factors are considered to determine reconstructive technique following mastectomy, such as need for adjuvant radiotherapy, breast size, degree of breast ptosis, comorbidities, age, and patient preference are used to determine the ideal post-mastectomy reconstructive approach in each patient (15-18). Some patients may even choose not to undergo post-mastectomy breast reconstruction given the risks of additional complications that a second surgery may impose. Reconstructive complications may delay adjuvant treatments; in TNBC, which inherently carries an increased risk of locoregional recurrence, this can greatly affect oncological outcomes (12). Overall, little is known about the outcomes of TNBC patients undergoing reconstruction, and no study to date has evaluated and compared the objective clinical factors associated with the decision to undergo implant versus autologous reconstruction in the TNBC population. Thus, the aim of this study is to evaluate the clinical factors that impact choice of post-mastectomy reconstructive technique in patients with TNBC, as well as to assess post-reconstruction surgical and oncologic outcomes in these high-risk patients. We present the following article in accordance with the STROBE reporting checklist (available at https://tbcr.amegroups.com/article/view/10.21037/tbcr-22-42/rc).
Methods
Following institutional review board approval (MHRI No. 00004330), a single institution retrospective chart review was performed for patients with TNBC who underwent post-mastectomy breast reconstruction from 2010 to 2020. TNBC patients who did not undergo post-mastectomy breast reconstruction were excluded. Patients over the age of 18 with biopsy-confirmed TNBC who underwent total mastectomy with reconstruction were included. Collected patient characteristics included demographics such as age, race, body mass index (BMI), smoking history, and other comorbidities such as diabetes or connective tissue disease. Breast cancer history was additionally collected, including details regarding cancer histology, tumor size and stage, and receipt of treatments such as chemotherapy or radiation therapy. Reconstruction was performed by multiple surgeons at this single institution. Patients were categorized depending on the initial post-mastectomy reconstructive technique they underwent: ABR or IBR. ABR included free tissue transfer or rotational/local flap reconstruction, while IBR included tissue expanders (TE) and saline or silicone implants. Additional details regarding follow-up procedures were also collected, such as mean months between TE and final reconstruction and the type of final reconstruction (ABR vs. IBR) that the patient received. Mean follow-up was described for ABR and IBR patients. Collected outcomes data comprised of rates of TNBC recurrence, postoperative complications, and mortality in the included patients.
Comparative analyses included patients who underwent ABR or IBR. STATA version 17.0 (StataCorp, College Station, TX) was used to conduct univariate Chi-square, Fisher’s exact, and paired t-tests to analyze the data for statistical significance, defined at values of P<0.05. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by institutional review board of MedStar Health Research Institute (No. 00004330) and individual consent for this retrospective analysis was waived.
Results
A total of 465 female patients were diagnosed with TNBC during the 10-year study period, of which 240 underwent total mastectomy. From these patients, 52.9% (n=127) underwent breast reconstruction. Reconstructive techniques most commonly included IBR (n=108, 85.0%), followed by ABR (n=19, 15.0%). Trends in reconstructive techniques performed for patients treated at our institution can be seen plotted over the past decade in Figure 1, which demonstrates an increase in ABR procedures over recent years. On average, patients who elected for ABR were older than patients undergoing IBR (54.3±10.4 vs. 46.4±10.9 years; P=0.040). There was no difference in race for patients who underwent ABR versus IBR (P=0.566), with 51.2% of those undergoing the procedures being Caucasian (n=64), 34.4% African American (n=43), 5.6% Asian (n=7), and 2.4% Hispanic or Latino (n=3). Patients with a higher BMI were more likely to undergo ABR compared to IBR (30.0 vs. 26.1 kg/m2; P=0.007). Patients with a current or prior smoking history were more likely to undergo ABR compared to IBR, though this was not significant (42.1% vs. 23.6%, P=0.092). Comorbidities, such as diabetes or connective tissue disease did not significantly influence choice of reconstruction type. Patient demographics for those who underwent ABR or IBR are summarized in Table 1.
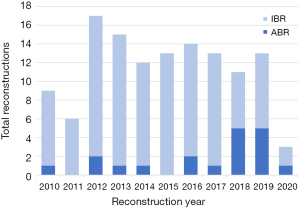
Table 1
| Variable | ABR + IBR reconstructions | ABR | IBR | P value |
|---|---|---|---|---|
| Total | 127 | 19 (15.0) | 108 (85.0) | – |
| Age, years | 47.8±11.3 | 54.3±10.4 | 46.4±10.9 | 0.040 |
| Racea | 0.566 | |||
| Caucasian | 64 (51.2) | 8 (44.4) | 56 (52.3) | |
| African American | 43 (34.4) | 9 (50.0) | 34 (31.8) | |
| Asian | 7 (5.6) | 1 (5.6) | 6 (5.6) | |
| Hispanic or Latino | 3 (2.4) | 0 (0.0) | 3 (2.8) | |
| Other | 8 (6.4) | 0 (0.0) | 8 (7.5) | |
| BMI, kg/m2 | 26.6±6.1 | 30.0±4.0 | 26.1±6.2 | 0.007 |
| Smoking historya | 33 (26.4) | 8 (42.1) | 25 (23.6) | 0.092 |
| Comorbidities | ||||
| Diabetesb | 4 (3.4) | 1 (5.3) | 3 (2.8) | 0.484 |
| Connective tissue diseasea | 4 (3.2) | 0 (0.0) | 4 (3.8) | 1.000 |
Data are shown as mean ± standard deviation or number (percentage). a, n=125; b, n=126. ABR, autologous-based reconstruction; IBR, implant-based reconstruction; BMI, body mass index.
Patients were more likely to undergo ABR compared to IBR if they had prior history of any type of breast cancer (36.8% vs. 16.7%; P=0.041) or if they experienced a TNBC recurrence (26.3% vs. 9.3%; P=0.034), while patients experiencing a primary occurrence of TNBC more often underwent IBR (90.7% vs. 73.7%; P=0.034). The trend to undergo ABR over IBR in patients with a prior history of breast surgery (i.e., lumpectomy, partial mastectomy, or cosmetic breast implant surgery) was not significant (42.1% vs. 23.1%; P=0.087). Patients with larger tumors tended to undergo IBR (2.4±1.6 cm2) compared to ABR (1.7±1.2 cm2), though this was not significant (P=0.085). Cancer histology and tumor stage at presentation had no influence on reconstruction choice. History of neoadjuvant versus adjuvant chemotherapy or radiation also had no effect on type of breast reconstruction chosen. Cancer characteristics stratified by type of reconstruction can be found in Table 2.
Table 2
| Variable | ABR + IBR reconstructions (n=127) | ABR (n=19) | IBR (n=108) | P value |
|---|---|---|---|---|
| Prior BC history | 25 (19.7) | 7 (36.8) | 18 (16.7) | 0.041 |
| Occurrence | 0.034 | |||
| Primary TNBC | 112 (88.2) | 14 (73.7) | 98 (90.7) | |
| Recurrence | 15 (11.8) | 5 (26.3) | 10 (9.3) | |
| Prior breast surgery | 33 (26.0) | 8 (42.1) | 25 (23.1) | 0.087 |
| Cancer histology | 0.066 | |||
| DCIS | 4 (3.2) | 0 (0.0) | 4 (3.7) | |
| Invasive ductal CA | 115 (90.6) | 16 (84. 2) | 99 (91.7) | |
| Invasive lobular CA | 2 (1.6) | 0 (0.0) | 2 (1.9) | |
| Mammary CA | 4 (3.2) | 3 (15.8) | 1 (0.9) | |
| Other | 2 (1.6) | 0 (0.0) | 2 (1.9) | |
| Tumor size (cm2)a | 2.3±1.6 | 1.7±1.2 | 2.4±1.6 | 0.085 |
| Tumor stageb | 0.640 | |||
| 0 | 2 (1.8) | 0 (0.0) | 2 (2.0) | |
| 1 | 39 (34.5) | 6 (40.0) | 33 (33.7) | |
| 2 | 58 (51.3) | 6 (40.0) | 52 (53.1) | |
| 3 | 13 (11.5) | 3 (20.0) | 10 (10.2) | |
| 4 | 1 (0.9) | 0 (0.0) | 1 (1.0) | |
| Chemotherapyc | 0.430 | |||
| Neoadjuvant | 47 (40.2) | 7 (46.7) | 40 (39.2) | |
| Adjuvant | 66 (56.4) | 7 (46.7) | 59 (57.8) | |
| Both | 4 (3.4) | 1 (6.7) | 3 (2.9) | |
| Radiation | – | |||
| Neoadjuvant | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Adjuvant | 40 (31.5) | 6 (33.3) | 34 (31.5) |
Data are shown as mean ± standard deviation or number (percentage). a, n=121; b, n=113; c, n=117. ABR, autologous-based reconstruction; IBR, implant-based reconstruction; BC, breast cancer; TNBC, triple negative breast cancers; CA, carcinoma.
At the time of primary oncologic surgery, 73.3% of patients (n=96) underwent contralateral mastectomy. Of these 96 patients, 3.1% (n=3) underwent mastectomy due to breast cancer in the contralateral breast, while 96.9% (n=93) underwent prophylactic contralateral mastectomy. All patients underwent reconstruction in the contralateral breast following mastectomy, with the majority undergoing the same reconstructive technique as in the primary breast (P<0.001). Patients undergoing IBR had longer follow-up compared to those undergoing ABR (54.7±33.7 vs. 32.9±24.9 months; P=0.006). Reconstructive outcomes such as complication rates were similar between cohorts. At mean follow-up of 51.4 months (range, 2.7–131.4 months), oncologic outcomes, such as TNBC recurrence and mortality rate, did not significantly differ between the two groups. Surgical outcomes and reconstructive details such as implant type used and time to final reconstruction following TE use are outlined in Table 3.
Table 3
| Variable | ABR + IBR reconstructions (n=127) | ABR (n=19) | IBR (n=108) | P value |
|---|---|---|---|---|
| Operative details | ||||
| Contralateral reconstruction technique | 96 | 13 | 83 | <0.001 |
| ABR | 12 (12.5) | 12 (92.3) | 0 (0.0) | |
| IBR | 81 (84.4) | 1 (7.7) | 80 (96.4) | |
| Implant-based reconstruction | – | – | – | |
| Tissue expander | 77 (71.3) | |||
| Silicone or saline implant | 31 (28.7) | |||
| Final reconstruction following TE | – | – | – | |
| <3 months | 10 (14.5) | |||
| 3–6 months | 26 (37.7) | |||
| 6–9 months | 12 (17.4) | |||
| 9–12 months | 12 (17.4) | |||
| 12–15 months | 6 (8.7) | |||
| >15 months | 3 (4.4) | |||
| Type of final reconstruction following TE | – | – | – | |
| ABR | 11 (15.9) | |||
| IBR | 58 (84.1) | |||
| Follow-up, months | 51.3±33.5 | 32.9±24.9 | 54.7±33.7 | 0.006 |
| Reconstructive and oncologic outcomes | ||||
| Recurrence | 17 (15.9) | 3 (15.8) | 14 (13.0) | 0.719 |
| Complications | 24 (19.1) | 6 (31.6) | 18 (16.8) | 0.131 |
| Mortality | 7 (5.6) | 0 (0.0) | 7 (6.5) | 0.593 |
Data are shown as mean ± standard deviation or number (percentage). ABR, autologous-based reconstruction; IBR, implant-based reconstruction; TE, tissue expander.
Discussion
This is the first study to evaluate post-mastectomy reconstruction methods specific to TNBC patients. Compared to an overall post-mastectomy reconstruction rate of 42% for all breast cancer patients (19), we report a higher rate of 52.9% within patients with TNBC. We found that compared to patients who underwent IBR, TNBC patients who underwent ABR were significantly older, had a higher BMI, and either had a prior history of breast cancer or experienced TNBC recurrence. Despite concerns for increased complication rates or locoregional recurrence in TNBC patients undergoing ABR, there was no significant difference in recurrence or mortality outcomes following ABR versus IBR techniques.
Butz et al. previously reported a significantly higher risk of 30-day postoperative complications in older patients receiving ABR compared to younger patients (20). Although ABR may confer greater operative risks in older patients due to longer operative times under general anesthesia, there are also reports that demonstrate no increased risk of complications in this cohort, which parallels our findings (21). Additionally, previous data has suggested that older women who opted for autologous reconstruction reported significantly higher satisfaction than women of the same age who underwent implant-based methods, in part because autologous reconstruction provides better symmetry (21). This may explain why a higher proportion of older patients chose to undergo ABR following mastectomy in our study (P=0.040).
Patients receiving autologous reconstruction had significantly higher BMI than those receiving IBR (P=0.007), suggesting that those with higher fat content may opt to use their own adipose tissue for breast reconstruction for the benefit of improving their body contour. Interestingly, there is mixed data regarding outcomes following ABR versus IBR in obese women, with some sources demonstrating increased complication rates in autologous reconstruction and other sources suggesting decreased complications and higher patient satisfaction with ABR (22,23). Furthermore, our data demonstrates no significant difference in complication rates between all women receiving ABR versus IBR. While an increase in BMI does pose a greater risk of postsurgical complications in general, this heterogeneity in reported outcomes from ABR warrants further investigation, and the decision to undergo certain reconstructive procedures should be based on clinical decision-making on a case-by-case basis.
It is well-known that smoking has an important deleterious impact on wound healing, and several reports have shown that nicotine use contributes to poor outcomes in both autologous and implant-based breast reconstruction (24-26). While not significant, there was a trend towards undergoing ABR in patients with a smoking history compared to those who underwent IBR (P=0.092). While the reason for this tendency is not entirely clear, it may prompt clinical providers to consider smoking history in reconstructive choice, given that the microvascular disease found in smokers may result in complications such as abdominal dehiscence. Larger studies are warranted to compare outcomes in smokers receiving ABR versus IBR in TNBC patients receiving breast reconstruction.
We found that patients with a personal history of breast cancer or recurrence were more likely to undergo ABR over IBR (P=0.041 and P=0.034, respectively). This corresponded to the trend towards undergoing ABR more commonly in those with a prior history of breast surgery (P=0.087), such as in cases of patients who underwent oncologic procedures for prior breast cancer. It has been previously reported that ABR is associated with higher cancer recurrence rates compared to those who undergo mastectomy alone, possibly due to extensive surgery activating dormant micrometastases, but more recent reports suggest that there is no increased recurrence risk (27). Importantly, our results suggest no difference in TNBC-specific recurrence following either ABR or IBR, paralleling other reports that have shown no association between breast reconstruction type and cancer recurrence (28). Our findings support that the relationship between personal breast cancer history, recurrence, and reconstructive choice is not causative. We also show that there is neither an increased risk of complications or mortality in patients who receive either autologous or implant-based reconstruction. These findings can provide invaluable information to patients who are often uncertain when choosing a particular reconstructive option, helping to ease the decision-making process by reducing concern for surgical or oncologic complications.
We report a greater percentage of TNBC patients undergoing reconstruction (52.9%) compared to what has previously been reported in the literature for all BC patients (42%) (19). This could be the result of patients being seen at a high-volume, tertiary academic center, and therefore may not reflect access to reconstruction nationally for TNBC patients, particularly in rural areas. Our institution saw an increase in the proportion of TNBC patients who received ABR in recent years compared to IBR. In 2018, 45.5% of TNBC breast reconstructions performed were autologous (Figure 1). This is compared to the period of 2010 to 2017, during which the average rate of ABR was only 7.7%. This significant increase in ABR is due to greater surgical experience and the addition of reconstructive microsurgeons who perform ABR at our center. Furthermore, the increase in ABR in the last few years may be due, in part, to recent reports linking textured breast implants to anaplastic large cell lymphoma (ALCL) and a greater awareness of illness related to breast implants, although currently unsubstantiated by evidence (29-31). Women have previously reported a fear of implants as a reason to forego reconstruction, despite the proven safety of this reconstructive method (32-34).
Strengths of this study include the 10-year study duration, allowing for a widespread evaluation of cases and trends at our institution. Inherent limitations of this study include a relatively small sample size. Thus, a larger study possibly utilizing a national dataset may provide a deeper understanding of demographic and medical factors that influence TNBC patients’ decision-making for post-mastectomy reconstruction. Second, our retrospective chart review study design depends on the quality of data reported within patients’ medical records. Additionally, an understanding of factors influencing TNBC patients’ decisions to undergo post-mastectomy reconstruction could not be achieved, due to non-reconstruction patients not being included in this study. While the aim of this study was to provide an overview of reconstructive methods and resulting outcomes in TNBC patients, a major limitation is the lack of details regarding the discussions and decisions made between surgeons and patients on choosing either autologous or implant-based reconstruction. Because both surgeon-sided and patient-sided factors influence this decision, further details would improve the conclusions found in this study; however, the long duration of this study and the heterogeneity in reconstructive surgeons make finding surgeon-sided decision-making rationales difficult to identify. Regardless of this limitation, no other study has identified the objective clinical factors that are associated with different modalities of breast reconstruction in TNBC patients, and this data could help guide physicians and patients better understand reconstructive options and outcomes. It would also be valuable to assess patient preferences to undergo reconstruction using a prospective survey of those who did and did not undergo the procedure to assess aspects affecting their decisions. Additionally, it would be interesting to compare TNBC reconstructive techniques to patients with other cancer subtypes to better appreciate any differences. Finally, based on our original classification of patients into ABR versus IBR groups, many patients who initially received TEs were included within IBR. Of these patients, 11 (15.9%) underwent eventual ABR, but were still considered within the IBR group due the patient classification system used for this study.
Conclusions
In patients with TNBC, the decision to undergo breast reconstruction should be based on the primary goal of a safe operative and oncologic outcome. In TNBC women undergoing reconstruction, older age, higher BMI, and a prior history of breast cancer were factors associated with undergoing ABR. Regardless of the reconstructive option undergone, we found no differences in recurrence, complications, or mortality in these high-risk TNBC patients. These findings provide valuable information to patients and physicians and may assist in the risk stratification component of the decision-making process.
Acknowledgments
We would like to thank our statistician, Eshetu Tefera.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://tbcr.amegroups.com/article/view/10.21037/tbcr-22-42/rc
Data Sharing Statement: Available at https://tbcr.amegroups.com/article/view/10.21037/tbcr-22-42/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tbcr.amegroups.com/article/view/10.21037/tbcr-22-42/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by institutional review board of MedStar Health Research Institute (No. 00004330) and individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Foulkes WD, Smith IE, Reis-Filho JS. Triple-negative breast cancer. N Engl J Med 2010;363:1938-48. [Crossref] [PubMed]
- Kumar P, Aggarwal R. An overview of triple-negative breast cancer. Arch Gynecol Obstet 2016;293:247-69. [Crossref] [PubMed]
- Dent R, Trudeau M, Pritchard KI, et al. Triple-negative breast cancer: clinical features and patterns of recurrence. Clin Cancer Res 2007;13:4429-34. [Crossref] [PubMed]
- Fancellu A, Houssami N, Sanna V, et al. Outcomes after breast-conserving surgery or mastectomy in patients with triple-negative breast cancer: meta-analysis. Br J Surg 2021;108:760-8. [Crossref] [PubMed]
- Chen QX, Wang XX, Lin PY, et al. The different outcomes between breast-conserving surgery and mastectomy in triple-negative breast cancer: a population-based study from the SEER 18 database. Oncotarget 2017;8:4773-80. [Crossref] [PubMed]
- Lowery AJ, Kell MR, Glynn RW, et al. Locoregional recurrence after breast cancer surgery: a systematic review by receptor phenotype. Breast Cancer Res Treat 2012;133:831-41. [Crossref] [PubMed]
- Golshan M, Cirrincione CT, Sikov WM, et al. Impact of neoadjuvant chemotherapy in stage II-III triple negative breast cancer on eligibility for breast-conserving surgery and breast conservation rates: surgical results from CALGB 40603 (Alliance). Ann Surg 2015;262:434-9; discussion 438-9. [Crossref] [PubMed]
- Gabos Z, Thoms J, Ghosh S, et al. The association between biological subtype and locoregional recurrence in newly diagnosed breast cancer. Breast Cancer Res Treat 2010;124:187-94. [Crossref] [PubMed]
- Elder EE, Brandberg Y, Björklund T, et al. Quality of life and patient satisfaction in breast cancer patients after immediate breast reconstruction: a prospective study. Breast 2005;14:201-8. [Crossref] [PubMed]
- Howard MA, Polo K, Pusic AL, et al. Breast cancer local recurrence after mastectomy and TRAM flap reconstruction: incidence and treatment options. Plast Reconstr Surg 2006;117:1381-6. [Crossref] [PubMed]
- Gieni M, Avram R, Dickson L, et al. Local breast cancer recurrence after mastectomy and immediate breast reconstruction for invasive cancer: a meta-analysis. Breast 2012;21:230-6. [Crossref] [PubMed]
- Grigor E, Stein M, Arnaout A, et al. Outcomes of Immediate Breast Reconstruction in Triple Negative Breast Cancer. Plast Reconstr Surg Glob Open 2021;9:28-9. [Crossref]
- Kneubil MC, Brollo J, Botteri E, et al. Breast cancer subtype approximations and loco-regional recurrence after immediate breast reconstruction. Eur J Surg Oncol 2013;39:260-5. [Crossref] [PubMed]
- Ha JH, Hong KY, Lee HB, et al. Oncologic outcomes after immediate breast reconstruction following mastectomy: comparison of implant and flap using propensity score matching. BMC Cancer 2020;20:78. [Crossref] [PubMed]
- Hidalgo DA, Borgen PJ, Petrek JA, et al. Immediate reconstruction after complete skin-sparing mastectomy with autologous tissue. J Am Coll Surg 1998;187:17-21. [Crossref] [PubMed]
- Nelson JA, Disa JJ. Breast Reconstruction and Radiation Therapy: An Update. Plast Reconstr Surg 2017;140:60S-8S. [Crossref] [PubMed]
- El-Sabawi B, Sosin M, Carey JN, et al. Breast reconstruction and adjuvant therapy: A systematic review of surgical outcomes. J Surg Oncol 2015;112:458-64. [Crossref] [PubMed]
- Carlson GW. Breast reconstruction. Surgical options and patient selection. Cancer 1994;74:436-9. [Crossref] [PubMed]
- Morrow M, Li Y, Alderman AK, et al. Access to breast reconstruction after mastectomy and patient perspectives on reconstruction decision making. JAMA Surg 2014;149:1015-21. [Crossref] [PubMed]
- Butz DR, Lapin B, Yao K, et al. Advanced age is a predictor of 30-day complications after autologous but not implant-based postmastectomy breast reconstruction. Plast Reconstr Surg 2015;135:253e-61e. [Crossref] [PubMed]
- Santosa KB, Qi J, Kim HM, et al. Effect of Patient Age on Outcomes in Breast Reconstruction: Results from a Multicenter Prospective Study. J Am Coll Surg 2016;223:745-54. [Crossref] [PubMed]
- Hanwright PJ, Davila AA, Hirsch EM, et al. The differential effect of BMI on prosthetic versus autogenous breast reconstruction: a multivariate analysis of 12,986 patients. Breast 2013;22:938-45. [Crossref] [PubMed]
- Klement KA, Hijjawi JB, LoGiudice JA, et al. Microsurgical Breast Reconstruction in the Obese: A Better Option Than Tissue Expander/Implant Reconstruction? Plast Reconstr Surg 2019;144:539-46. [Crossref] [PubMed]
- Klasson S, Nyman J, Svensson H, et al. Smoking increases donor site complications in breast reconstruction with DIEP flap. J Plast Surg Hand Surg 2016;50:331-5. [Crossref] [PubMed]
- Chang DW, Reece GP, Wang B, et al. Effect of smoking on complications in patients undergoing free TRAM flap breast reconstruction. Plast Reconstr Surg 2000;105:2374-80. [Crossref] [PubMed]
- Zucker I, Bouz A, Castro G, et al. Smoking as a Risk Factor for Surgical Site Complications in Implant-Based Breast Surgery. Cureus 2021;13:e18876. [Crossref] [PubMed]
- Svee A, Mani M, Sandquist K, et al. Survival and risk of breast cancer recurrence after breast reconstruction with deep inferior epigastric perforator flap. Br J Surg 2018;105:1446-53. [Crossref] [PubMed]
- Ha JH, Hong KY, Lee HB, et al. Oncologic outcomes after immediate breast reconstruction following mastectomy: comparison of implant and flap using propensity score matching. BMC Cancer 2020;20:78. [Crossref] [PubMed]
- Leberfinger AN, Behar BJ, Williams NC, et al. Breast Implant-Associated Anaplastic Large Cell Lymphoma: A Systematic Review. JAMA Surg 2017;152:1161-8. [Crossref] [PubMed]
- Magnusson MR, Cooter RD, Rakhorst H, et al. Breast Implant Illness: A Way Forward. Plast Reconstr Surg 2019;143:74S-81S. [Crossref] [PubMed]
- Newby JM, Tang S, Faasse K, et al. Commentary on: Understanding Breast Implant Illness. Aesthet Surg J 2021;41:1367-79. [Crossref] [PubMed]
- McCarthy CM, Pusic AL, Sclafani L, et al. Breast cancer recurrence following prosthetic, postmastectomy reconstruction: incidence, detection, and treatment. Plast Reconstr Surg 2008;121:381-8. [Crossref] [PubMed]
- Eriksen C, Frisell J, Wickman M, et al. Immediate reconstruction with implants in women with invasive breast cancer does not affect oncological safety in a matched cohort study. Breast Cancer Res Treat 2011;127:439-46. [Crossref] [PubMed]
- Bezuhly M, Temple C, Sigurdson LJ, et al. Immediate postmastectomy reconstruction is associated with improved breast cancer-specific survival: evidence and new challenges from the Surveillance, Epidemiology, and End Results database. Cancer 2009;115:4648-54. [Crossref] [PubMed]
Cite this article as: Sayyed AA, Towfighi P, Deldar R, Aminpour N, Sogunro O, Maini M, Masanam M, Son JD, Fan KL, Song DH. A retrospective cohort study comparing reconstructive techniques and outcomes in post-mastectomy triple negative breast cancer patients. Transl Breast Cancer Res 2023;4:5.


